“Resisting Callousness in health care: a role for spirituality”
NAJC Plenary Session
January 18, 2017
Thank you very much, to all of you for inviting me to this conference. Thank you especially, Dr. Katz and Dr. Weiner, for introducing me to this group of warm and brilliant people. As some of you know, I am a bit nervous about speaking to a group whose work is so different from what I have done for the past 35 years. I believe we will find many areas where our hopes and efforts to relieve suffering can intersect.
My topic is Resisting Callousness in Health Care. I will try to make a case that awareness of spirituality, particularly a spirituality of compassion, is important in health care. But to be able to bring it to bear, we have to resist the callousness that results from the hidden effects of greed, anger and delusion.
Let me introduce myself for a few minutes, trying to explain how I come to stand before you to share these experiences and thoughts. I was given 90 minutes, and I believe I could fill all the time with my words. I think I won’t and instead we should make time for a bit of a conversation. If at the end of this time, we can learn how to do the work of health care more compassionately and generously, then we will have done something to change our paradigms.
It is my thesis today that what we encounter in hospitals and health care is, at basis, suffering: health care is distinguished from other industries as an industry that always encounters loss, decline and death – out of which suffering must follow. The industry generally fails to acknowledge it or confront it, but suffering is present in many forms. On some days I feel I am surrounded by it – in our patients, but also in our colleagues. We can choose to build compassion (the wish to relieve suffering), or we can choose to become calloused and hard-hearted.
The failure to acknowledge and address the presence of suffering, especially when combined with the paradigms of industry, makes for callousness. I took a sabbatical from medicine in 2013 to overcome my burn-out then: I felt then I would either lose my mind, or lose my soul.
I will also try to turn this conversation toward how change must begin within oneself – by becoming aware of causes of suffering and callousness, and how change must also occur in institutions in order for change to be lasting. All of this is informed by my understanding that “spirituality” matters: spirituality comes from awareness that we are transient and destined for sorrow and losses, and that we can choose to find comfort as well as purpose in being connected to one another. There is a wonder and a miracle in how we can lessen our pains by being present for one another and by sharing in our joys and sorrows.
How does a Chinese-American, Christian physician chat with a batch of Jewish chaplains? Let me explain myself.
- I was born in NY in 1953, the first son of a first son of Chinese immigrants. My father was an engineer and culturally a Confucian Chinese; he married an independent-minded woman who had worked as a journalist in WWII. They underwent immigration hardships during the McCarthy times, and eventually found stability and opportunity to fit in. My dad worked his whole life at IBM; my mom raised us three kids, then in 1979 re-connected with her wartime contacts in China (now the PRC), early after China was “opened” again.
- As part of my upbringing, I was raised in a Christian household – Riverside Church in NYC was a stalwart part of my parents’ support in their time of immigration crisis. I went to good schools, and eventually ended up in pulmonary and critical care medicine. In 2012 I took advantage of the option to grandfather into Palliative Care. I have two grown children. I have been at Rochester General Hospital since 1990, and have witnessed the rise of more and more industrialized medical care in that time.
- By 2012 I was also feeling tremendous dissatisfaction in medical practice. Electronic records were being introduced, and the conflict between the professional and mercenary aspects of medicine was getting more noticeable. I felt in danger of losing my mind or losing my soul. I decided to take (give myself) a sabbatical, and went to Union Theological Seminary in New York in the spring of 2013.
- The questions I hoped to explore were: first, why does religion seem unnecessary for some, but insufficient for others to deal with the suffering of death and dying; second, what has been said about suffering and how do we recognize and respond to it?
- Union is a liberal Protestant seminary, and my courses there were intellectually challenging, and spiritually invigorating. I had courses taught by former priests and by Buddhist-Christian double belongers. I learned Zen meditation, and also studied Ignatian (Jesuit) meditation. I learned about Paul, the former Jewish rabbi who taught that the Jewish God could also be worshipped by gentiles – Christ created a pathway of freedom that resisted the religion of submission required by the Roman occupation. One of my courses was about Abraham Joshua Heschel, and the professor was Cornel West. While I was there, there was a conference on Christian-Buddhist dialogue. I unfortunately did not have much exposure to Hinduism or Islam.
Clearly the idea that one religion can have all the answers is impossibly naive. In a global world, inter-religious dialogue will be necessary, even when agreement is not possible.
- I returned to Rochester, and slowly have tried to create a role for myself that can combine my clinical and spiritual sides. I believe that the experiences of health care may be informing us of the limitations of ignoring the spiritual side of experience. Maybe the frustration with medicine as business and industry is telling us to attend to other ways that we must interact with each other.
- This audience offers a new challenge to me. When I speak to my medical colleagues, I sense they may feel I am “out there” in my attention to non-technical aspects of medicine, but I can use my status and experience in their field to stretch and push them in new directions. With your field, I do not have status and my only experience is novice. I can only ground my comments in my medical experience, and hope to provoke curiosity about the connections I have observed between that world and the world you inhabit.
- Preparing this talk has helped me further my own development as well. I am at an age when Jung would say that I am trying to find my vocation more fully. Giving voice to these ideas has helped me harmonize the strands of knowledge and experience that I have accumulated. Let’s see if they can resonate with some of yours.
Before we proceed, we should define how I use the terms I will discuss.
Spirituality for this discussion is a sense of connectedness to something beyond Self. Such self-transcendent awareness will also tend to encourage a connectedness to other persons. It often will be a source of purpose and meaning, but is it also adequate as a source of support in the face of suffering? Our mortality and the necessary sorrows that accompany it, I propose, can be powerful reminders of connectedness. We all share in suffering. But connectedness alone may not be enough. I would hope also that there would be a sense of wonder accompanying the sense of connectedness. Rabbi Heschel warned that losing the sense of wonder could be dangerous: “dazzled by the brilliant achievements of the intellect in science and technique, we [can be] deluded into believing that we are the masters of the earth and our will the ultimate criterion of what is right and wrong.” It helps to retain a sense of wonder; not to do so might be “a sign of a half-hearted, listless mind, of an undeveloped sense for the depth of things” (Not Alone, 21).
Suffering is an experience common to all sentient life. Its study and definition have not received much interest in the medical literature, because it is not measurable in its parts or as a whole. Dr. Eric Cassell in his seminal article “The Nature of Suffering and the Goals of Medicine” (N Eng J Med 1982; 306:639-45) defined it as “the state of severe distress associated with events that threaten the intactness of the person.” (I am not sure the word “severe” is even necessary, as there are manifestations of suffering that are tolerable, familiar and chronic, but still constitute suffering.) It is a state of Mind, and it originates in an individual’s manner of personhood. We will discuss something of Dr. Cassell’s definitions and descriptions. It is important to realize that he warns against reductionist methods that might de-construct suffering into dimensions that allow measurement and observation.
“Compassion” I will refer to as the wish to relieve someone’s suffering. It is thus somewhat different than “empathy” and also different from loving kindness. The latter (loving kindness) besides wishing a relief of suffering, also hopes for and promotes the happiness of another. The former (empathy) involves being able to appreciate another person’s emotional state, and to experience those emotions as one’s own. It is interesting to note that functional MRI seems to identify different areas of brain activation for empathy and compassion. And it is even more notable that loving-kindness meditation (LKM) can enhance activation of brain regions associated with compassion and empathy, and can also increase altruistic behaviors in psychological testing! We are far from understanding how different areas of the brain interact to process reception, reasoning and impulse generation. My wish would be to always maintain wonder at the complexity of Mind, and not allow experimental “evidence” to over-simplify or negate the holistic appreciation of Experience. Who we are and what we do are not reducible to what we can measure, think or express in words.
If I were to make a generalization about how end of life experiences could be used to encourage a sense of spirituality, I would emphasize that aging and illness will include uncertainty, suffering, and multiple losses: not just the losses of physical function and comfort, but also the pain of loneliness, and especially the pain of leaving and separating. There is also the risk of losing a sense of meaning.
It becomes a matter of choice and intent whether awareness of that suffering will lead to empathy and compassion, or … to its opposite, callousness, hardness of heart. How we approach suffering provides us with insights into how to avoid callousness. That in the end is the more important aspect of encouraging awareness of suffering and connectedness.
How do we approach suffering? I venture to say that it is a question that is avoided – in health care, and in American life.
In our fortunate modern American lives, there are relatively few opportunities to address suffering. As a result, there is little practice in recognizing and approaching uncertainty, sorrow and loss. It is an observation of neuroscience that physical comfort and a sense of emotional well-being can actually reduce empathy and reduce awareness of others’ suffering. When a culture distracts from and denies suffering, it might “help” individuals deal with their own sorrows and losses, but it detracts from those individuals being available for the support of others. I would submit that a culture that promotes delusion, one that encourages material and temporal attachments, and that denies anger will discourage compassion and foster callousness.
Our fortunate modern American lives encourage a spirituality of optimistic resistance to negative emotions and situational setbacks. We tend to believe that there is little that cannot be overcome with perseverance, money and hope. (It is foundational in America: life, liberty and the pursuit of happiness are our unalienable rights.) When confronting natural and man-made disasters, this type of spirituality promotes individual fortitude and communal solidarity – there are losses to overcome, resolutions to be made; there is little time or will to spend on mourning and acceptance. We are most familiar with this spirituality, as we see it after football game losses, weather disasters, and 9/11. We tend to believe that with more perseverance, money and hope, anything can be overcome.
Such events challenge us with their randomness and unpredictability, but they are generally self-contained and even temporary. Ill-health, on the other hand, will be a given for all of us – universally, and eventually finally. In health care, therefore, some kind of suffering will always present: I believe it is where we collect and concentrate encounters with uncertainty, decline, loss and death. The spirituality of optimism, the familiar spirituality, is still called on to engage the suffering of ill-health. But it may not serve us well.
As we introduce a public discussion of spirituality, I believe there will come better awareness of types of spirituality. First of all, the spirituality that we use to overcome adversity while in health may not be the only one to use, especially in the presence of ill-health. Perhaps that is the most important distinction to acknowledge. But even in the presence of the suffering of illness, there may be different aspects to spirituality. For instance, the spirituality of compassion that I will encourage for health care workers and health care institutions does not coincide with the spiritualities that patients and families will have to summon for their support and meaning. We can and should invite questions and discussions of how individuals and institutions understand and address suffering. We can and should try to understand and resist sources of callousness. But … we will not find one prescription or solution for all situations and individuals. This is an age-old challenge that has not found a universal answer yet. We have to maintain respect for the diversity of solutions, even as we insist on confronting the reality of the questions.
I want to build toward how we might resist callousness. First we need to analyze and discuss suffering in health care. I believe this is where I can provide my best input, as I have seen much patient care, and I continue to marvel at the many ways patients and providers approach their illnesses. I will not discuss much about empathy except to recognize its value. As I have said, I prefer to emphasize the role of compassion. I will approach it in a somewhat negative way: by discussing how we are thwarted by desires, hidden anger and delusions. If we can resist these sources of callousness, I believe we will gradually be able to be more compassionate. It is the work of many lives: As we know, paraphrasing the familiar words of Rabbi Tarfon: “The day is short and the work is endless … [We] are not required to complete the work, but neither are [we] free to desist from it.”
Life contains suffering – it is an empirical observation. It is delusional to imagine that suffering will be someone else’s lot, and never one’s own.
Suffering in illness occurs when we feel damaged, “un-whole.” How much suffering accompanies loss depends on whether other aspects of selfhood are adequate to sustain us. So I might be able to tolerate an amputation or a colostomy, if I had adequate connection to my friends, my work, my books, whatever. We always need Something Else to support us when we mourn a loss.
The relief of physical suffering is the job of effective medical care, a task that is necessary always. We of course know that the task of symptom relief is one we too often fail to achieve. I cannot go into details there, except to say it is often not a matter of knowledge and skills, but one of attitude. It is frustrating to feel powerless, so we sometimes avoid the most complex situations. But importantly, physical discomfort is not the only source of suffering. I want to note three other important kinds of suffering that can burden patients and families, and their care providers: the anxiety created by uncertainty, the pain of leaving, and the pain of losing one’s sense of meaning.
Uncertainty
A patient of mine always feared she would develop lung cancer, and then she did – incurable, advanced, but somewhat treatable. Do we emphasize the treatable aspect, and ignore or deny the incurability? Or emphasize that treatments are not curative, might extend her life by months, and come with side-effects? How do we accompany patients starting on their path of terminal illness? When is “hope” false hope? What is hope?
These are only some of the questions that patients and families face. As a physician, I believe I can be vague and non-committal about these metaphysical questions. I hope and imagine that you as chaplains have aptitude and attitude enough to engage these patients and their loved ones. But I also imagine you folks want us folks to provide the grounding in certainty.
I would group the anxiety caused by uncertainty with other types of pain. How one deals with uncertainty will tell us much about the person – whether she is goal-directed primarily, or able to abide in moments; whether she is able to allow events to run their courses, or she needs to retain strict control; whether she has support and self-esteem, or is adrift and influenced by circumstances.
Leaving
Leaving also hurts. It is remarkable how powerful the wish can be for more time together. It is hard enough to say I’m sorry and I forgive you; it is really hard to say good-bye. I believe it is the pain and fear of being left alone – sometimes for the patient, sometimes for the family – that so attaches the dying to their suffering at the end of life. I believe we have seen patients who prefer the familiarity of physical suffering to the strangeness of dying and being left alone. There are no easy answers to this feeling that leaving is finally done alone. Is this one of the reasons religions evolved? I would be curious to hear what you say to your patients and yourselves about this mystery – why do we feel alone in our passing on?
Loss of meaning
Finally, the loss of a sense of meaning can also be tragic. When faced with illness, the question of “Why me?” is frequent. Issues of meaning and connectedness may not arise while we are in health. But one’s faith and beliefs will be tested once challenged by illness, aging or impending loss. I bring up these issues because it seems we spend too much energy, time and resources avoiding this most basic of questions: why was I put here? The endings of life can remind us how to live life. My answer, in general, is that we need to build awareness of our transience and of our connectedness. And then we need to try to relieve the suffering that we encounter.
For better and for worse, I am resigned that illness and death will not be banished from the most perfect of worlds. Suffering is one of the experiences that unites us, perhaps the most important experience that unites us. It is harsh to say to someone facing a terminal illness – “What did you expect, not to suffer?” But we can challenge ourselves while still in health to begin to consider that difficult question.
“I am human; nothing human is foreign to me.” Suffering is universal, and perhaps that realization can help to ease feelings of being especially unfortunate when it is our turn. In fact I believe we need to assume that every patient has her own ways of suffering and coping. The fact that we do not assume there is suffering or seek its particular expressions illustrates our callousness. Let’s look at our callousness together.
Callousness has become a laudable virtue in health care culture – a fact of life. Even if it is not encouraged, callousness is defended. I witnessed this recently as I (naively) tried to discuss post-mortem care with nurses (wrapping bodies). I had hoped that we might encourage more empathy and compassion in physicians by encouraging attending physicians and residents to join nurses in this final common pathway of our patients – which of course we will share also. (How many of you have participated?) I imagined that the ritual behind closed doors – after all the technology had stopped – was one that humanized nurses in a way that no physician would ever know. After all, for physicians our first encounter with bodies is in gross anatomy, and our recurrent encounters used to be around autopsies. The tactile experience with cold and blue bodies might be a simple reminder of our ultimate empty-handedness and fragile humanity. In order to understand the process, I asked to assist nurses in our ICU with one of their patients.
Boy, what a romantic idea my idea turned out to be. Modern day hospitals do not disrespect the bodies of the deceased, but there was little or no reflection or emotional content in the process. The body was there, cold and bluish, but there was no ritual of washing or preparing. The body was stripped, but not re-wrapped in clean garments. A toe tag was placed, and there was a pre-prepared white plastic bag for the transport to the morgue. The body was rolled into the bag, as if the person was included as part of a final bed linen change. Nurses often will delegate this task to patient care technicians. It’s a matter of tagging and bagging, one nurse said. Another acknowledged that there was sadness, but sadness that could not and should not be fully experienced. She stated matter-of-factly that one becomes automatically calloused to the routine. And she asked, not unkindly, what did I expect – some kind of spiritual experience?
What is wrong with this picture? Is anything wrong with this picture? If (as some have stated) how we treat the dead reflects how we care for the living, what have I learned from this encounter with callousness regarded as virtue? Indeed, this encounter does inform us about how we care for the living: in health care these days, we care for them efficiently, dispassionately, and without regard or awareness of our connectedness to them. Individually and collectively in health care we callous and distract ourselves from possibilities for compassion.
“Health is everything” has become a mantra. “If you don’t have your health, you don’t have anything” is a cliché; it short-changes everyone who comes down with a major or even a minor illness. The emptiness implied in these statements is the reason we are here today. We might ask how such an unexamined sentiment has become so ingrained in the common psyche.
In the dance with the entropy of Nature, there used to be acknowledgement that eventually Mother Nature would win, and that part of the dance involved preparations by the individual and the community for a good death. The main part of health care now has to do with restoring bodily functions (parts of bodies), even if the repairing and patching produce only partial or temporary respite. Offering drugs and devices to prevent and restore a semblance of health is easier than counseling patients about limitations and desiring less. It is marketed, and the expectation is created that drugs and devices must be tried – death and disability are only a final option. So health care has become an industry mostly about delaying illness and death, not about alleviating suffering or supporting compassion.
Institutionally there is great self-interest in avoiding honest discussion of the limits of health care. It is easier and more profitable for institutions to offer procedures that appeal to the desires of patients: a joint replacement that might or might not relieve pain; a catheterization that might or might not relieve uncertainty. New services are “revenue streams.” But it defers to someone else the inevitable need to discuss mortality and cost. The goal of increasing individual and institutional revenue generally tips the balance in favor of doing more.
For individual patients, the options of doing more and hoping for the best will almost always defeat the opposite strategy: to accept limits, engage in the support of suffering, and not prolong dying in bits and pieces. Even if they can approach serious illnesses with philosophical acceptance, patients are often cajoled by families and physicians to accept more suffering in the hopes that more days can be found.
So hospitals fill up with the acutely ill, and clinics with the chronically ill; those who used to die at 70 live till 80 and beyond; there are more and more ill persons needing care. The industry of health care has promoted the idea that more life and more health are always possible. Unfortunately this misrepresents the limits of biology, and it leaves our patients and our staffs ill-prepared for the time when there are no more options to try. If you have nothing if you do not have health, and eventually you will lose your health – then the logic is that eventually you will have nothing. How do we counteract that logic?
Let’s look back on what I believe I just described. In health care, as illustrated in my experience with the wrapping of bodies, there is increasing emphasis on efficiency. That followed from the objectives of generating revenue, measuring processes and outcomes, and cutting costs. All of this detracts from the recognition of the presence of suffering in patients.
Here we can borrow fruitfully from Buddhism. I have found it useful to use the analysis that behind most of our suffering lie Greed, Anger and Delusion. Borrowing use of these categories has helped me to find explanations for why we fail so often to offer compassion: our greed, anger and delusions.
What Dr. Eric Cassell (“Nature of Suffering and the Goals of Medicine”) had to say about suffering relates in close fashion to what Buddhists included under Greed. The term Greed includes not only the wishes to gain material things excessively. Greed or Craving or Attachment also include wishes not to lose things of value. Isn’t that what Dr. Cassell was referring to? When we lose dimensions of selfhood (it doesn’t have to be physical only) – e.g. losing physical comfort, income, vocational ability, social relations, sense of status and worth, emotional stability, sense of certainty etc. – there is possibility of “suffering.” I have emphasized that ill-health will eventually force on us the need to lose and leave much of what we value and accumulate. The more we cannot adjust to losses, the more likely there will be suffering.
For health care workers and health care institutions, there are also ample examples of how Greed relates to callousness. We have just discussed how the marketing of desires increases desires. The expectation that there will always be a drug or a device to relieve ill-health combines both Delusion and Craving. The costs of health care rise, of course, because no one wants to lose income (nurses, physicians, administrators, salespeople, drug companies, stockholders, regulators, even chaplains). If we wish to encourage compassion, we have to become aware of and address our wishes to have more and not to lose what we have. Insight into this universal trait can help us resist callousness, but changing our practices will be still be a great challenge. When we search for Greed, it is always there to be found.
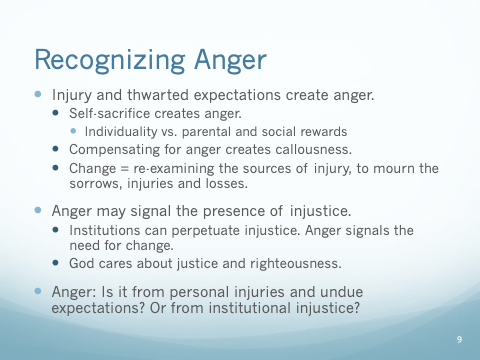
Recognizing Anger as a barrier to compassion is particularly useful, in my opinion, though also very difficult. Allow me a few minutes to develop ideas about anger, and then to illustrate its effects in health care.
Anger results from injury and thwarted expectations, so it is related to Craving in a way, the desire not to lose something of value. Others relate Anger to a sense of injustice – but that still begs the question if the expectation of justice is something to hold onto, or something to let go of. Either way, anger necessitates defenses because we are generally taught that anger needs to be channeled effectively.
To limit the effects of anger, one first needs insight: to search for injuries and to examine expectations. But insight is not enough. There needs to be efforts to grieve and then to live differently: we need good support to examine and mourn our sorrows, losses and thwarted expectations, and we need models and practice in changing our responses. Unexamined anger influences behaviors, often in ways that isolate us emotionally and spiritually from others. This is the work of psychology and counseling. It is helpful and perhaps necessary work that I would support for anyone who works in a helping profession – help yourself with your baggage.
My own therapy has helped me understand better (and still not completely) how defenses against anger can produce effective and productive behaviors, yet also damage my ability to live authentically. Self-sacrifice in the service to others can be celebrated and rewarded as virtuous, but it is still self-sacrifice.
Sacrificing of self takes its tolls. My father’s Confucian upbringing held that parents must teach children how to conform to the ways of the world. My Western and Christian upbringing in contrast, allows me to say that I also have my uniqueness to answer for. In America we not only have our unique genetic and physical fingerprints, but we believe our individuality contains something true about ourselves that no one else can fully share or know.
Each personality has a history of desires and defenses; it has had learned and taught expectations. Whatever it takes to find one’s True Self, it is often not what our parents wished for us, or what the world required. From early years onward there were many ways we were taught to deal with anger. Too often there can be denial and doubting of anger: “don’t be mad.” As children we learn to take on the values of others in order not to feel conflict (internalization). Once reason can be employed to balance the emotions, we can use intellectualization. We channel anger toward “productive” behaviors – sublimation and compensation are identified as mature defense mechanisms. I believe it is not a far reach to suggest that the rewards of riches, status, and pride are compensatory for many hidden injuries. These rewards are … rewarding. But successful hardening to one’s own injuries will also make it more difficult to see similar struggles and pains in others. The theme today is how to build our awareness of suffering, and the barriers to alleviating it. Compensating for anger is one great barrier.
And not all anger is undesirable: anger is also an important signal of injury and thwarted expectation that have resulted from injustice. In the Christian-Buddhist dialogue conference at Union in 2013, it was very instructive to watch experts in the two religions approach each other on the issue of anger. The Buddhists reminded their Christian counterparts that without addressing manifestations of anger (as well as craving and delusion) in oneself, it is difficult to engage in compassionate work to relieve suffering in others. Change must begin within oneself. The Christian participants reminded their counterparts that suffering does not only exist because of personal issues: institutions also perpetuate suffering. Governments, businesses, churches and even monasteries can perpetuate suffering. When there is systemic suffering, it is not enough to change one’s mind; it is also important to work for just social solutions. The internal and the external environments both need attention to relieve suffering.
When I seek out behaviors that mask anger, I believe I see them as pervasive and self-perpetuating. My compulsiveness and inability to leave work until I am exhausted physically, mentally, emotionally: I have learned to feel virtuous in being able to meet demands at the expense of my own needs. And, since I know it’s possible for me, I expect others to strive for my ideals.
Nurses become calloused by unexpressed anger over patients’ and families’ demands (demands originating from the patients’ own losses), and calloused by physicians’ anger masking as competitiveness, greed, intellectual arrogance and personal narcissism.
Young physicians are sacrificing their current needs in order to meet the performance requirements of their training. It takes great discipline and resilience to work through hours/days/years of fatigue, anxiety, fear, and sadness, never mind the judgments and abuse from a few nurses, teachers or patients who fail to appreciate the efforts they are making, and that they are doing their best. It takes great discipline to do all that is required. We generally deny that injuries and losses have occurred, and we rarely discuss or process them.
Everyone in the helping professions has deferred personal pleasure and personal goals. Becoming “professional” implies self-sacrifice: we have to become self-motivated, dutiful and persevering. I do not question the necessity of the kinds of experiences that have served as rites of passage, and they have their rewards. I do challenge the practice of never re-examining those defining moments. Even after we have pulled ourselves together to forget about it, get over it, and move on, we can still return later on to re-examine those formative professional moments that contribute to our hidden anger and callousness.
There are also many systemic causes for anger. Who has the power to define the content of conversations? Why is the financial bottom line, the bottom line? Change has to occur, often without our ability to influence those changes. But do the systems we work in care enough to explain and support the “team,” tweak the system to make it more humane, and resist the insinuations imposed by government and insurers; or does it seek only to game the system for its fiscal well-being? It is proper to feel anger when the ability to provide compassionate care, and to relieve suffering is at stake.
I wonder, is this something rabbis and pastors also experience? Do you suppress personal wishes in order to meet professional expectations? Are those expectations fully integrated into your psyches, or do they still need compensations (in riches, status or pride)?
There does need to be assessment of where the anger is coming from: if it is from the accumulation of losses and insults that relate to patients’ suffering, then we have ourselves to work on. But if the anger is from institutional callousness, then there can and should be criticism of systems that imagine our roles to be reliable, efficient, dispassionate distributors of standardized health care. Intelligent robots might some day do that kind of work better than we can. But it would be a hard-hearted system. Isn’t that something to get angry about?
Rabbi Heschel centers his book The Prophets on the divine pathos – it is in God’s nature to care about mankind. Included in that is the fact that God is not indifferent to evil. Justice and its expressions in compassion and righteousness are God’s purposes in history. We are our brothers’ keepers; few may be guilty, but all are responsible; indifference to the wrongs done to other people is an evil. Evil begins in exceptional behaviors, and becomes terrible when the exceptional is allowed to be acceptable. Anger becomes a symptom and signal that injury has been done to us and to those around us. We should not acquiesce to it through delusion or escape into spirituality that is only sentimentality.
Concluding this section: The anger aspect of callousness begins prior to going to professional school. It begins in the sacrifice of personal goals in favor of parental and social values: work hard, get ahead, succeed, get past it, move on. Callousness is reinforced every time a painful experience is repressed in the interest of duty, or when an opportunity to examine one’s own or someone else’s suffering is neglected or avoided. We lose connections to ourselves and others when we deny that feelings matter and compassion matters. We become calloused when we hide anger at the unfairness of a system that does not allow time and support to process what we see in fellow humans and what we do to them. And we become more calloused because we cannot be angry about it. Callousness becomes automatic, as long as we try again and again to get past the feelings and move on.
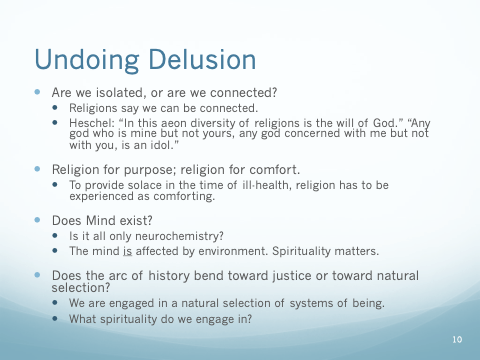
I suspect though that even if we knew how to deal with our desires and defenses, it still would not be enough to build compassion and empathy for patients, families and colleagues. Here there is a philosophical, but also an experiential challenge: are we isolated in our identities, or are we connected in our relatedness? Do we subscribe to, teach and model a spirituality of empathy, compassion and collaboration, or do we believe the world is one of competition and natural selection?
Modern American life does not offer many opportunities to discuss “spirituality.” These issues are complex and contradictory: otherwise we would have easy solutions that we could all agree on. The complexity discourages reflection and discourse, but we are here today to rejuvenate our desire and courage to continue with the struggle and the discussion.
When I took my sabbatical, you might recall, I was wondering why religion did not seem necessary for some, and for others it was not sufficient to help them let go of life. I believe I have an answer that helps me. I believe the words Religion and Spirituality apply to different and overlapping functions. One role of religion is to explain and teach behaviors that are shared by a community of adherents. Religions are parts of socialization; faith beliefs provide purpose and structures to our lives. The other role of religion and spirituality parallels and reinforces the pre-verbal experiences of infancy. Such pre-verbal experiences support our abilities to trust, hope and love. As we lose our lifelong gains in mastery, health and function, it is these aspects of spirituality and religion that we will need to sustain us.
The great religions address these issues. But for end of life issues, we need to focus on the comfort aspect of religion, not the purpose part. The Jewish response, from my limited encounter with Rabbi Heschel, seems to be to understand that beyond all the mystery and pain there is a God who cares, and the purpose of living is to play one’s part in that understanding: we should care for widows and orphans because God cares for justice and righteousness.
The Christian idea seems to extend that, making Christ’s life and teachings an example of how nothing can separate us from the steadfastness of God’s love. At the time of the writing of the New Testament, Rome had destroyed the Temple, and Christians were hounded for their beliefs – but even in that violent and power-driven world, there could be knowledge of the peace of Christ.
It seems that the Buddhist idea is that our current incarnation is only our latest effort to see through the illusions of consciousness in order to understand the connectedness and interdependence of being.
One function of religion and spirituality is to extend one’s perspective – to see beyond one’s own suffering to understand the universality of that type of experience. Religions have tried to provide reasons not to live in isolation – but it is still left to us to embody their systems of belief and reasoning. They have tried to provide means to understand intellectually, feel emotionally and live practically within a shared humanity: there are ways to respond to injury besides anger and isolation.
But even if one does not subscribe to any formal religion (with their bureaucracies and systems), one can still come to know that sorrow is “the deepest thing,” a thread that exists within all human experience. Knowing, feeling and sharing such awareness, we might have less anger over our individually perceived injuries, and more sympathy, empathy or compassion for the struggles of others.
Scientific Rationalism would have us believe otherwise. Medicine prides itself on its scientific and technological prowess. It offers its segregation from religion and spirituality as one of the reasons for its success. Neuroscience is discovering and marveling at the interactions that are made through neurons and biochemistry. As scientists glimpse how symbols and emotions and memories interact, there may develop a hubris that when they discover enough about the workings of the brain, they might understand the workings of the Mind. It might then seem unnecessary to appreciate beauty, model empathy, behave bravely, and love selflessly. Spirit could be explained by biology. Who would need religions, if they seemed only to justify violence and segregation? Who would need spirituality if we could feel at one with others through chemistry and pharmacology?
I wonder if that vision has not already been included in someone’s grant proposal! But to get to that utopian state we would still need spiritual awareness and moral guidance. Even if we could manipulate behaviors with drugs, it would still be necessary to define what behaviors to encourage. Would we still want to evolve toward justice and compassion, for instance?
The failed political movements of the 20th century showed that social and political structures could not survive if they did not value the idea of personal freedom. We are embarking on another era of challenge: do we believe in the idea that warmth of human relationship matters. The current model seems to assume that individuals and societies are economic entities seeking to optimize wealth and power. The arc of history, this model seems to suggest, does not bend toward justice, but toward survival of the fittest. The extension (or perhaps the requirement) is that the parts of the whole would also behave with similar economic self-interest.
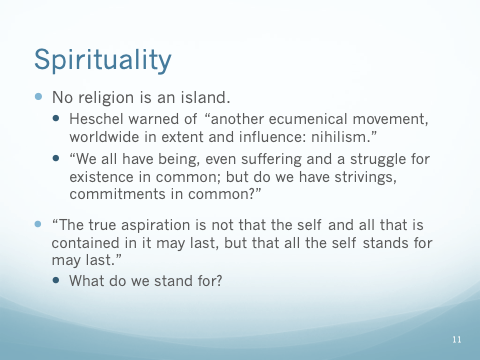
These are examples of what Rabbi Heschel warned us of 50 years ago. He said in his great address in 1965, “No Religion is an Island” that there is “another ecumenical movement, worldwide in extent and influence: nihilism” (Moral Grandeur, 237). Nihilism has only grown since then. The idea that our time together is based on competition and self-interest can seem even “logical” at times. After all, our behaviors seem to originate in combinations of biochemistry that do not rely on meaning and purpose: they can seem arbitrary, and merely contingent on input. The concept of natural selection is ingrained in our liberal thinking. I would suggest though that the natural selection we are now part of is the natural selection of systems of being – of the types of spirituality that we engage in. Our words and our ideas and our interactions matter now more than ever, because that is what now influences evolution, not the survival of individual specimens of humanity. Even if the elements of our brains that control behavior could be understood, the environment still matters: The mind as a “transitory combination of elements borrowed from the environment” still depends on the environment, including the culture and spirituality of it. (Tom Wolfe, Jefferson Lecture, 2006)
The experiences of ill-health remind us, if we care to observe and be reminded, that our influences on each other are not fluky, and they are not even extinguished when a life ends. How we see ourselves in relation to others can be absorbed uncritically from the environment, or we could alter it conscientiously through changes in our institutions and ourselves. Let’s continue a discussion of spirituality by observing how patients and families grope personally with the questions of meaning and connection that have challenged our ancestors, challenge our peers, and will challenge our descendants.
At Rochester General Hospital we have a joke about severe illness: in France, death is considered a tragedy, and in England it’s a duty. But, in America it’s considered an option. Not a tragedy or a duty, death is (sort of) an option. Here is where we have to discuss spirituality. It is the part of the discussion where we tackle our connections to each other.
For millennia death was a tragedy, and it was evident that individuals were powerless before natural forces: Shakespeare said “like flies to wanton boys are we to the gods: they kill us for sport.” With our technologies we can delude ourselves into believing that the circumstances have changed. Medical science has been guilty of encouraging that delusion – that death is an option. But if it is a delusion, who should be responsible for disenchanting us?
In some countries there is acceptance that there will be limits because resources are finite. It takes a village to raise a child, but it also takes a village to sustain a life in decline. At some point in some societies, there becomes a duty to accept the village’s limits. How do we create villages where persons know each other, trust each other, care for each other enough to feel it is part of citizenship not to demand endlessly of others?
We seem to be in a phase where the “marketplace” is a mysterious, unconscious arbiter. Belief in the “marketplace” is a kind of spirituality: it is an extension of concepts of natural selection and economics based on individuality and competition. There is an idea that economic prosperity might result in generosity and charity. But that is not the ideal. Creating an ideal of generosity and charity will take self-examination and practice, and a sense of what kind of connectedness to strive for.
In a country of prosperity and materialism, there is the habit that objects can comfort us, and they do seem to express or comfort aspects of Self. Rabbi Heschel knew better: in the 1960s he wrote, “Imagine how smug, complacent, vapid, and foolish we would be if we had to subsist on prosperity alone.” The reality of aging and illness proves that all the objects we gain will have to be given up sooner or later. Will we suffer then, or will we be prepared with other supports?
Triumphing over adversity is an American archetype. We live in a country of opportunity and hope, and setbacks are regarded as challenges. Teachers and coaches teach that; performers and athletes model it.
This type of spirituality often will extend to the time of ill-health: we can pay for better opportunities, and we can hope. I recently took care of a family whose mother was coming to the end of years of struggle with ovarian cancer. I could and did offer to drain fluid from her chest to relieve her breathing – it didn’t help much. She had failed chemotherapy in Philadelphia through Cancer Treatment Centers of America; she hoped to go to Buffalo’s Roswell Park Cancer Institute to see if they could provide some type of immunotherapy – the term conjures up thoughts of modern magic. She was struggling to get to the bathroom ten feet away, and she said she was hoping to get in a car to go to Buffalo. Why and how did she find strength to remain in denial? I asked her daughter-in-law, and she said it was because of her sons. What did her sons do? They were all wrestlers in high school; one still coached wrestling. In wrestling, one said, you never give up. We were able, with her husband’s support and perhaps with my nudging, to ask the men to see their mom’s physical and emotional exhaustion, to move away from their “hopes” based on perseverance, self-denial, and dream of medical miracles. Those were all wishes in the face of the realities. It was time to open their hearts to see the pain in someone they loved – the physical pain she suffered, and also the emotional and spiritual pain they shared in realizing their futures would not be together. Was there a chance to find some transcendent meaning? I don’t know. If a different meaning had been practiced (something besides the honor and pride of self-sacrifice), would it have helped to relieve the suffering of leaving? I don’t know.
We have many models of spirituality. They are absorbed from cultural influences around us, unexamined through lack of interest and from distraction by easy answers to difficult questions. There are other, examined models – they are called religions, but they cannot live and grow without attention to the environments they inhabit.
Rabbi Heschel warned long ago that religion had not declined because science had refuted it, but because it had become “irrelevant, dull, oppressive, insipid.” He challenged listeners then, and searchers now, with the observations that our humanity includes a sense of the ineffable – Something is “there” (out there and in there) that we cannot find through reason, measurement, and all our powers of “discursive thinking.” Those cognitive powers are immense, and they can seduce us into believing that we might master and grasp what it means to be human. Buddhists teach disciplined mind control to discard and delete concepts, feelings, sensations, impulses and even consciousness. The resulting Emptiness (paradoxically) enables experience of connectedness: so it seems possible that many aspects of personhood actually stand in the way of connectedness and interdependence.
Jews and Christians know of a God beyond human comprehension (“Any god who is mine but not yours, any god concerned with me but not with you, is an idol,” Rabbi Heschel warned). This God not only has been involved in history, sending words and persons to instruct, but this God remains concerned that humans live in concern for one another – justice, love and righteousness are connected.
No religion is an island, because they all seek to understand the mystery and miracle of what it means to live together. They demonstrate different understandings of that miracle and mystery. One religion cannot “reasonably” explain another one through its own terms. (We cannot “understand” Buddhism through Judeo-Christian reasoning.) But perhaps all religions need each other: “In this aeon diversity of religions is the will of God,” Rabbi Heschel noted. All religions stand against a different spirituality – one that says that we are random and meaningless fragments, molecules interacting (sometimes consumed, sometimes consuming) but without a purpose. Our glands and our minds would be enough to guide our interactions; our hearts would only circulate the blood.
Callousness would be OK if this were true. The callousness we see in health care raises spiritual issues. Should we be aware of the interests of others? Are our persons of a whole, or can we be de-constructed into our parts? How do our physical parts relate, and if we could support and sustain a damaged or aging part, is that good enough? “We all have being, even suffering and a struggle for existence in common; but do we have strivings, commitments in common?” (Not Alone, 105).
As I have said now several times, hospitals bring together and concentrate experiences of loss and suffering. Our professions seek to relieve that suffering, but in the end the suffering cannot be eliminated. We have to (kindly) remind those not in hospitals that their health is temporary; that ill-health awaits them as well. The uncertainties of ill-health provide opportunities to ask what we should do when we return to a semblance of certainty. And for those who have recovered from illness, when the pain of ill-health is temporarily relieved or the function temporarily restored, what do we live for then?
“I am human; nothing human is foreign to me.” Our shared predicament is that we find Truth buried; we see pain, greed and mystery whenever we look, though we prefer not to look. I do not find consolation in our predicaments, but I do try to take courage because for today there is a spark of God in me that I can be responsible for. And my comfort and meaning (my spirituality) is in knowing that when I mind that spark, when it is not distracted and dimmed by my desires and defenses (my cravings and anger), I am freer to see and say and do what I can to relieve the suffering of someone else.
I would like to conclude with Rabbi Heschel, of course. He wrote in 1951 (Man is Not Alone): “The true aspiration is not that the self and all that is contained in it may last, but that all that the self stands for may last.” The effort to understand what one stands for is a work of a lifetime, and the end of life is not soon enough to begin that effort.


